Have Good Health Insurance? Too Bad. You Could Still Get A $250,000 Bill
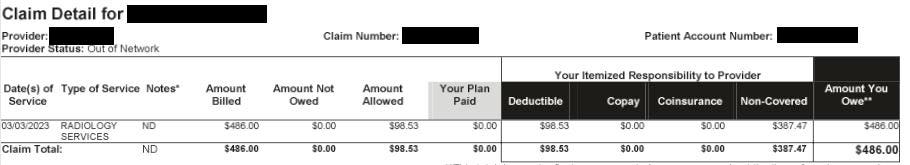
Generic “radiology services” claim from Jack’s insurance claim, with no other description provided. … [ ]
Former United States Surgeon General Jerome Adams recently tweeted his disbelief at being charged $4,896 for an ER visit for dehydration after hiking—and that’s after his insurance had settled its portion. If he struggles to understand why healthcare bills are so high, it doesn’t bode well for the rest of us.
As a professor of emergency medicine and health policy at the University of California San Francisco, I have spent over a decade researching our healthcare system and documenting the Wild West of hospital bills. It started when a friend in my neighborhood was hospitalized for appendicitis and was billed over $53,000. He asked me what a typical charge for appendicitis was, and after doing a little research, I found the charges for uncomplicated appendicitis cases ranged from $1,500 to $180,000.
Such ranges aren’t limited to surgeries; even routine cases like a normal vaginal delivery can be as low as $3,296 to as high as $37,227. These variations are even common in the most routine blood labs, with one hospital that charged more than $10,000 and another that charged $10 for the same cholesterol blood test.
Most of us who are fortunate to have insurance hope and feel shielded from these absurdities. Yet unfortunately that’s not the case. None of us—even if we are insured—is immune from the financially devastating effects of the administrative monstrosity of the U.S. healthcare system.
My friend Jack Emerson is an example of an educated, employed, dually insured American who is in this exact situation. He has been paying into Medicare his entire working life, for the past 40 years, and he and his employer also have been paying monthly premiums for private insurance.
Post-pandemic work for him and his company had been remote for years, and last March, they decided to have an all-company gathering in anticipation of an upcoming 50th-anniversary celebration. As Jack was on stage getting ready for a presentation, he suddenly had a cardiac arrest. Fortunately for him, the very public nature of his medical event meant that he received almost immediate CPR, and 911 brought him to the ER of Kaiser Redwood City, California, where he was admitted for six days and amazingly survived to tell his story. Sadly, his discharge from the hospital would be the beginning of what has been 10 months (and counting) of significant mental anxiety and stress for him due to the financial ramifications of a lack of communication between the hospital and his insurance companies.
Jack has the fortune of being covered by both Medicare Part A and employer health insurance through United Healthcare. The charges of his total hospitalization were over $250,000. Despite repeated inquiries to Kaiser, United Healthcare, and Medicare, it appears there are more than 30 outstanding claims that somehow have not been submitted or processed. As so many of us who have touched the healthcare system know, multiple phone calls by Jack to each of these entities have provided conflicting information with no definitive action.
A closer look at Jack’s hospital bills shows only the date of service, a generic description such as “inpatient visit,” and an even less descriptive disclosure of the provider (e.g., “Permanente Medical”). In some cases, there is a name of an actual provider, but again, no more description of what service it provided other than something like, “Diagnostic Services.” This is akin to us going to Safeway to buy bread, milk, and eggs, and the receipt we receive as “Food.” Except the charges, in this case, are astronomical.
In reviewing his claim summaries, I created an Excel spreadsheet so I could see them in one place. There are 55 of these esoteric and poorly described services in categories such as “inpatient visits,” “inpatient services,” “medical services,” and “diagnostic services.” Within “inpatient services,” three of the same services are listed with the same claim number and same dates of service but have been charged separately as $18,323, $58,408, and $99,508. There is no further description of what these “inpatient services” entail.
Amount billed for generically labeled “inpatient services” with same dates and same claim number but … [ ] different charges and no further information.
Is this a billing error? Or charges for different services? There is no way to know. Sadly, this lack of information on the statements is not particular to Kaiser; it’s just how things have been done and accepted in healthcare in the United States. While the next step will be for us to ask for itemized bills so we can clarify what he is actually being charged for, the entire process—even for me as a healthcare researcher who has dedicated her career to studying these issues—is exhausting. Imagine the burden it would place on someone who nearly died and is now recovering.
There is no other industry in the United States where we as Americans would tolerate such opacity in charges as well as ineptitude in dealing with them from service providers, whether they be the hospital or insurance companies.
How can we make sure we aren’t caught as powerless patients in this administrative web of complexity? On an individual level, each of us, upon receiving medical services, could embark on an emotionally draining and time-intensive endeavor to obtain our itemized bills and negotiate with the hospital and insurance company (or multiple ones, in some cases). But sadly, the likelihood of any success is low.
It is time we put our collective energies toward changing the referee-free zone of healthcare.
Recent policies have focused on price transparency, which 90% of Americans favor, with examples such as the Centers for Medicare and Medicaid Services Hospital Price Transparency rule and other current bills in Congress, such as S.3548 H.R. 4822 and H.R. 410, which would require cost transparency, including from insurers. There are legitimate concerns about potential unintended consequences of disclosing prices, which could include driving up prices (from hospitals that raise their prices to match competitors rather than decreasing them, as patients cannot act as true consumers). Yet while we don’t have all the answers, it is clear that the current status quo of “mystery prices” is not serving the public.
On a larger level, more fundamental reform that addresses the fragmented delivery and financing of healthcare care is needed. This is happening across the country in numerous states. California SB770, for example, was signed by Governor Gavin Newsom to start the process of creating a single-payer financing system across the state. There are also more incremental approaches of a “public option” that allow individuals to opt into a government-administered plan that competes with private plans. Washington and Colorado have operational public option-style programs (although using a non-traditional model of private insurers), and Nevada’s program is slated to launch in 2026.
While no program is perfect, we must change the system so we don’t continue to be victims of an expensive and inefficient system. Excess billing and insurance costs account for 15% of U.S. health spending. These costs do not translate to the provision of any healthcare services.
Overhauling our system would mean that the $350 billion annually we spend on excess billing and insurance administration could easily take care of the $195 billion of collective healthcare debt that 41% of Americans face.
As it stands, in the current system, if Jerome and Jack can’t figure out their healthcare bills and get them paid, we’re all screwed.